Acquired aplastic anemia (AA) is a bone marrow failure disease caused by T cell-mediated autoimmune attack on hematopoietic stem and progenitor cells (HSPCs). Identifying autoreactive T cells in AA has been challenging. Advances in T cell receptor (TCR) sequencing and the discovery of Human Leukocyte Antigen Class I (HLA-I) risk alleles linked to autoantigen presentation in AA have rekindled interest in exploring T cell repertoires in AA. We hypothesized that autoreactive CD8 + T cells in AA may have convergent TCR structures allowing them to recognize AA autoantigens presented by specific HLA-I risk alleles. To test our hypothesis, we analyzed TCR repertoires and HLA-restricted CD8 + T cell reactivity in AA patients.
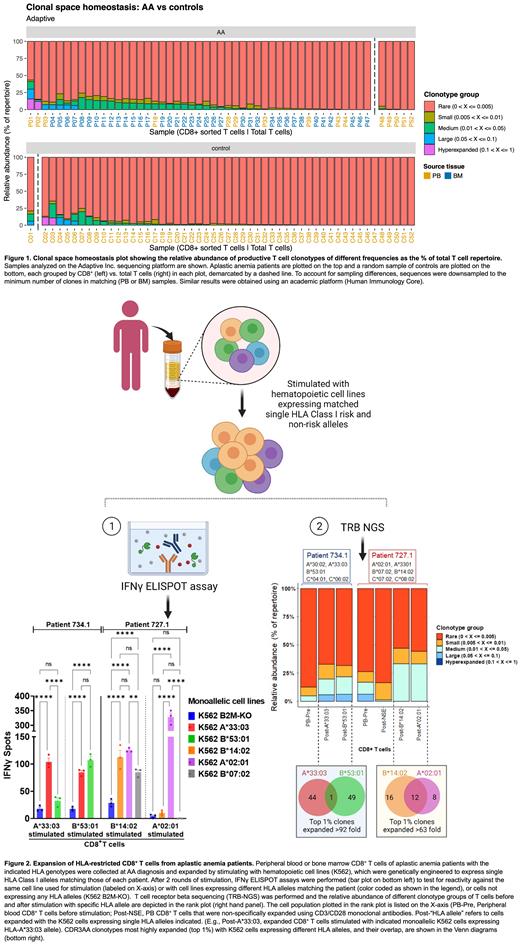
Using TCR Vβ (TRB) sequencing, we analyzed 83 patient samples obtained at AA diagnosis or relapse. High-risk alleles HLA-B*14:02 and B*40:02 were present in 26% and 10% of patients, respectively. HLA-DR*15 was present in 24%. Patient samples were largely sorted bone marrow (BM) CD8 + T lymphocytes. Patient TRB repertoires were compared to those in 709 control samples, largely of unsorted peripheral blood (PB). To account for sampling differences, we downsampled sequences to the minimum number of clones in the matching tissue. Normalized clone size distributions were visualized on rank plots (Fig 1).
TRB repertoires in both patients and controls were diverse. Highly expanded clones (>5%) were rare in either group. Patients had 1,415,069 unique CDR3 amino acid sequences (CDR3AA), of which 106,446 (7.5%) were shared by ≥2 patients. Among the 106,446 shared CDR3AA, 95.4% were found in controls, and 4.3% TCRs had reported specificity to exogenous (mostly viral) or endogenous antigens in VDJdb. 4,920 (4.6%) of the shared CDR3AA were detected only in patients (median 2 patients (2-25)). Of these, 190 exhibited TCR convergence in ≥1 patient, such that the same CDR3AA was encoded by ≥2 distinct nucleotide sequences. Clustering 4,920 patient-associated CDR3AA using GLIPH (Grouping of lymphocyte interactions by paratope hotspots) identified 43 TCR antigen convergence groups. CDR3AA in each cluster were not significantly expanded in the majority of patients and were not enriched for the high-risk alleles HLA-B*14:02 or B*40:02. Our data suggest that most CDR3AA in AA are private (unique to individual patients). Shared autoreactive CDR3AA may exist in patients but are likely to also be present in healthy individuals.
As the next step towards identifying autoreactive T cells, we focused on AA patients with known HLA-I risk alleles. We tested their CD8 + T cells for reactivity with endogenously expressed antigens by stimulating T cells with hematopoietic cell lines engineered to express single HLA-I alleles matching those of the patients (Fig 2). TRB sequencing showed increased clonality and significant expansion of a subset of clonotypes after T cell stimulation. Interferon γ enzyme-linked immunospot assays confirmed the expanded T cells' responsiveness to antigens presented by HLA alleles used for T cell stimulation. Additionally, these expanded T cells demonstrated variable reactivity to cells expressing other HLA alleles from the same patient. Among the 1% of CDR3AA clonotypes most highly expanded with single HLA-I alleles (63-3000-fold), we identified several that were expanded in an HLA-restricted manner. However, several highly expanded CDR3AA were highly expanded with multiple HLA alleles. Potential reasons for expansion of some CDR3AA after stimulation with cells expressing different HLA alleles include 1) binding of the same CDR3AA to different antigens presented by distinct HLA alleles, 2) expansion in response to the same antigens presented by distinct HLA alleles, or 3) expansion in response to non-HLA antigens.
In conclusion, our data show diverse and mostly private TRB repertoires in AA patients. Our in vitro findings suggest that much like T cell responses in non-AA individuals, T cell responses in AA are diverse and exhibit flexibility with respect to activation in response to various endogenous antigens in the context of different self HLA-I alleles. Given the diversity of TCR responses observed in AA patients, the tissue specificity of autoimmune attack and established association with risk HLA-I alleles in AA remain a mystery and likely require HSPC-specific autoantigen expression and efficient autoantigen presentation by individual patients' HLA-I alleles.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal